Our Assessment Pathway for Children and Families
We aim to make our assessment process clear, transparent, and supportive for children, young people, and their families.
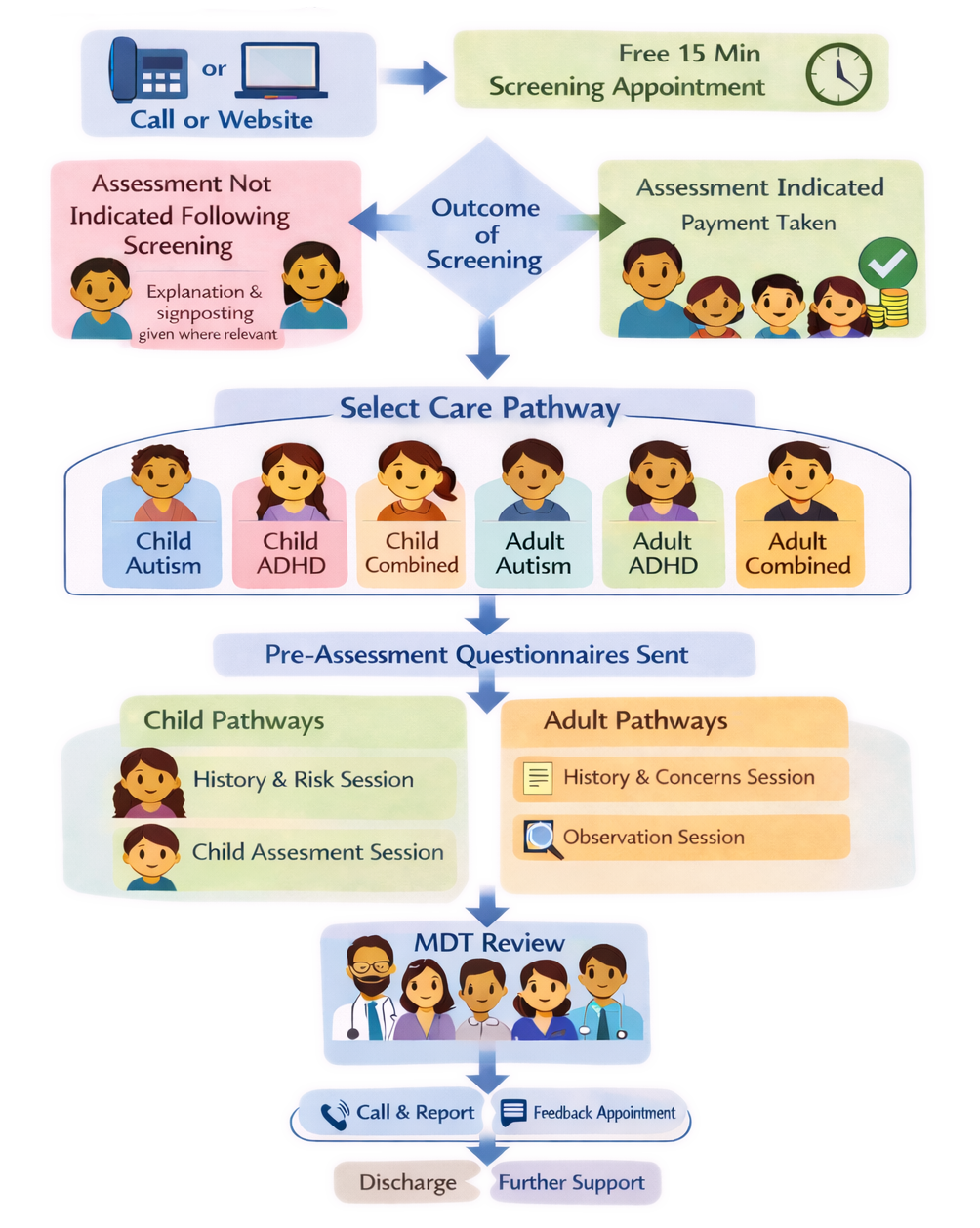
The pathway below outlines what typically happens from first contact through to assessment, feedback, and next steps.
Our assessments are not tests, and there are no right or wrong answers. We are not looking for children or young people to behave in a certain way. Our role is to understand their experiences so that appropriate support and recommendations can be offered.
01 A short screening
All families are offered a free 15-minute screening appointment. This appointment provides space to discuss current concerns, ask questions, and consider whether an assessment is indicated at this time.
Screening appointments are usually held with parents or carers. Children do not need to attend this appointment unless it is felt to be helpful.
We know that predictability is important for many children and families, and we aim to reduce surprises wherever possible.
If an assessment is not indicated following screening, this will be explained clearly, and alternative options or signposting may be discussed where appropriate.
If an assessment is indicated, payment is taken and the child or young person is placed on the most appropriate care pathway.
02 Preparing for assessment
Pre-assessment questionnaires are sent to families and reviewed by a senior clinician. The assessment process is informed by a multidisciplinary team with a range of professional backgrounds.
Families are provided with clear information about what will happen next, who will be involved, and how to prepare their child or young person for appointments.
We recognise that children and young people may feel anxious about assessment, and we encourage families to share any worries, preferences, or support needs in advance.
03 Child pathways
For children on child assessment pathways, the first appointment is a history and risk session. This session is held with parents or carers and focuses on early development, current concerns, and understanding the child’s needs.
Children do not need to attend this session. This helps ensure that children are not asked lots of detailed or adult-focused questions and allows clinicians to gather background information in a supportive way.
The second appointment is a child assessment session, which the child attends. Parents may attend for support if needed, but we ask that they do not answer questions on the child’s behalf.
04 Supporting the voice of children and young people
The voice of the child or young person is central to our assessments. We take time to listen carefully to their experiences, views, and preferences, using developmentally appropriate and flexible approaches.
As children grow older, their need for privacy, autonomy, and involvement in decisions often increases.
05 Supporting the voice of teenagers (aged 12 and over)
Teenagers are encouraged to be actively involved in their assessment and to share their views directly with clinicians.
Where appropriate, teenagers are invited to attend the initial part of the history session so that current concerns, consent, and any immediate risks can be discussed together. Parents or carers then provide developmental history separately.
We support young people to understand their rights around consent and confidentiality in a clear and age-appropriate way.
06 Assessment approach
Assessment sessions are adapted to suit the individual child or young person. This may include:
- breaks
- pacing sessions over more than one appointment
- use of visual or creative methods
- support from a parent or carer where helpful
We recognise that children, young people, and parents may sometimes have different views, and we take time to consider these carefully and respectfully.
07 Multidisciplinary team review
Once all assessment information has been gathered, it is reviewed by the multidisciplinary team. This allows perspectives from different professional backgrounds to be considered together.
08 Feedback and next steps
Families can choose how they receive feedback. This may include:
- an initial phone call with the outcome and written report shared, followed by a feedback appointment, or
- a feedback appointment where findings and recommendations are discussed together
Feedback sessions focus on understanding the assessment findings and agreeing appropriate next steps.
Following feedback, families may be discharged or offered further support options where appropriate.
Book Free Screening Appointment
Supporting your child - A guide for parents and carers
We encourage parents and carers to:
- talk openly with their child about what to expect
- use the child-facing pages and visual guides together
- reassure their child that there are no right or wrong answers
- let their child know that breaks and support are always available
Nothing will happen without children and young people being informed in a way that is right for them.
Children often have questions — sometimes directly, sometimes through behaviour or worries. This guide offers simple ways to answer common questions, using language that supports reassurance and predictability.
You don’t need to use these word-for-word. What matters most is keeping explanations simple, honest, and calm.
“Why are you talking to them?”
You might say: Grown-ups talk first so the clinician can understand things better and so you don’t have to answer lots of grown-up questions later.
“Am I in trouble?”
You might say: No. You haven’t done anything wrong. This is about helping grown-ups understand how to support you.
“Do I have to do this?”
You might say: You only join the sessions that are meant for you. We will tell you what’s happening before it happens.
“What if I don’t know what to say?”
You might say: That’s okay. There are no right or wrong answers. You can take your time or ask for help.
“Will they test me?”
You might say: It’s not a test. The clinician just wants to get to know you and understand how you think and feel.
“Who will I meet?”
You might say: You’ll meet a clinician on the screen. Some clinicians are doctors and some are not. They wear normal clothes and won’t examine your body.
“What if I feel nervous?”
You might say: Feeling nervous is okay. You can tell the clinician, ask for a break, or have me nearby. They will go at your pace.
“How long will it take?”
You might say: It will be about the same time as a lesson or a TV programme, and you can have breaks if you need them.
“What happens after?”
You might say: After the sessions, the clinicians talk together and then we’ll talk about what they’ve learned and how to help you.
Tips for supporting your child
- Read the child-facing page or visual guide together
- Keep explanations short — less is often more
- Repeat reassurance if needed (children often ask the same question more than once)
- Avoid giving too much detail about diagnoses or outcomes
- Let your child lead how much they want to talk
One helpful sentence to come back to
Many parents find it helpful to repeat this sentence:
Nothing will happen without you knowing, and you can ask questions at any time.
What Not to Say (and what to say instead)
This guide isn’t about getting things “right” all the time. It’s here to help avoid phrases that can increase worry or pressure, especially for children who are anxious or sensitive to uncertainty.
“Don’t worry”
Why this can be hard: It can make children feel their worry isn’t being heard.
Try instead: It’s okay to feel nervous. I’m here with you.
“They’re just going to check you”
Why this can be hard: “Check” can sound like something is wrong or being tested.
Try instead: They want to get to know you and understand how you think and feel.
“You have to answer their questions”
Why this can be hard: Creates pressure and fear of getting things wrong.
Try instead: You can take your time, and you can ask for help or a break.
“It’s really important”
Why this can be hard: Can increase fear of consequences or failure.
Try instead: We’re doing this to help understand you better.
“We’ll see what they decide”
Why this can be hard: Sounds like something is being done to the child.
Try instead: We’ll talk together about what they’ve learned and what might help.
“Just be yourself”
Why this can be hard: Can feel confusing or impossible under pressure.
Try instead: You can just be how you are today.
“You’ll be fine”
Why this can be hard: Can feel dismissive if the child feels nervous.
Try instead: I’ll be with you, and we can take breaks if you need them.
“It’s just a call”
Why this can be hard: Minimises feelings if the child finds calls difficult.
Try instead: We can make the call feel as comfortable as possible.
“Try your best”
Why this can be hard: Can sound like performance is expected.
Try instead: There are no right or wrong answers.
A helpful reminder for parents
Children often listen closely to tone as well as words.
Staying calm, predictable, and honest matters more than saying the “perfect” thing.
If you’re unsure what to say, it’s okay to say, "I don’t know yet, but we’ll find out together".